Turning on Testosterone: From the Mitochondria Up
Inside my self-experiment testing a new class of peptides that may boost testosterone by tuning the cell’s powerhouses.
Wait, Testosterone Starts in the Mitochondria?
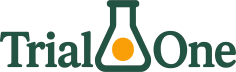
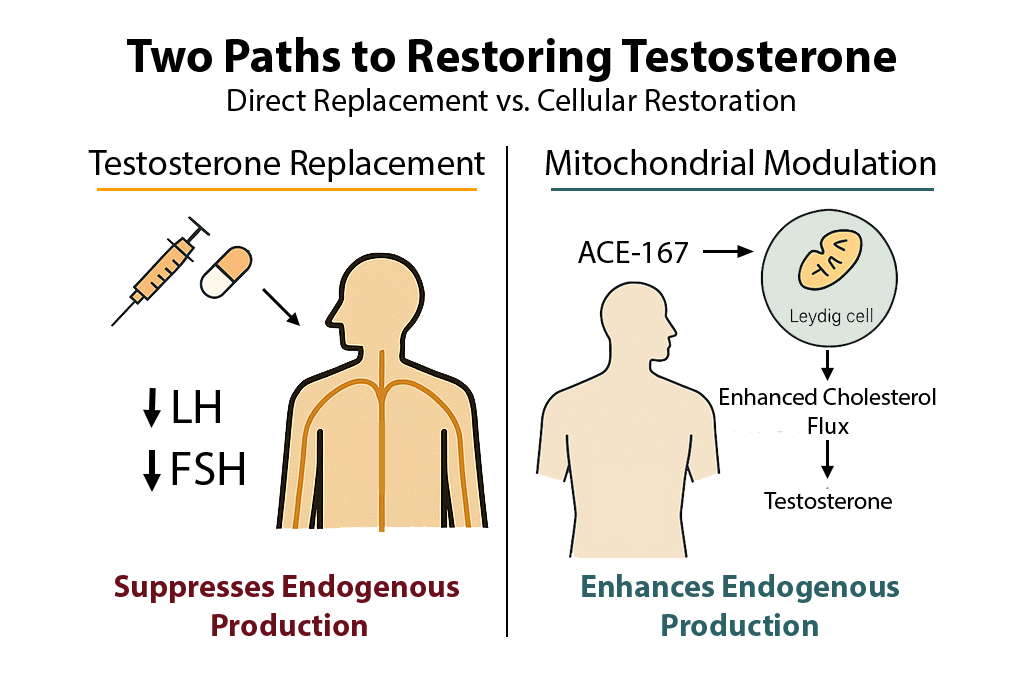
Most people think testosterone just… happens. But under the hood, every molecule of it begins life inside a small chemical factory called a mitochondrion, the same “powerhouse of the cell” you probably remember from biology class. Before testosterone can be made, cholesterol has to be transported into these mitochondria. That step is the gatekeeper of hormone production, and that’s where this story begins.
The Mitochondrial Gatekeeper: VDAC1
VDAC1 (Voltage-Dependent Anion Channel 1) is a molecular doorway that helps cholesterol move across the mitochondrial membrane. When it’s working efficiently, cells produce testosterone smoothly. When it’s held back by another protein called 14-3-3ε, that gate tightens and testosterone output can drop.
In rodent studies, disrupting that handshake between VDAC1 and 14-3-3ε caused a clear increase in testosterone, not from adding hormones, but from letting the body’s own machinery work more efficiently.
Meet the Peptides: ACE-167 and N163-166 Mod. 6
Small, stable peptide molecules have been engineered to mimic the part of VDAC1 that 14-3-3ε binds to. When injected, they act like a “decoy” that removes the brake on the system: unlocking cholesterol flow and boosting testosterone naturally.
Two candidates stood out from animal studies:
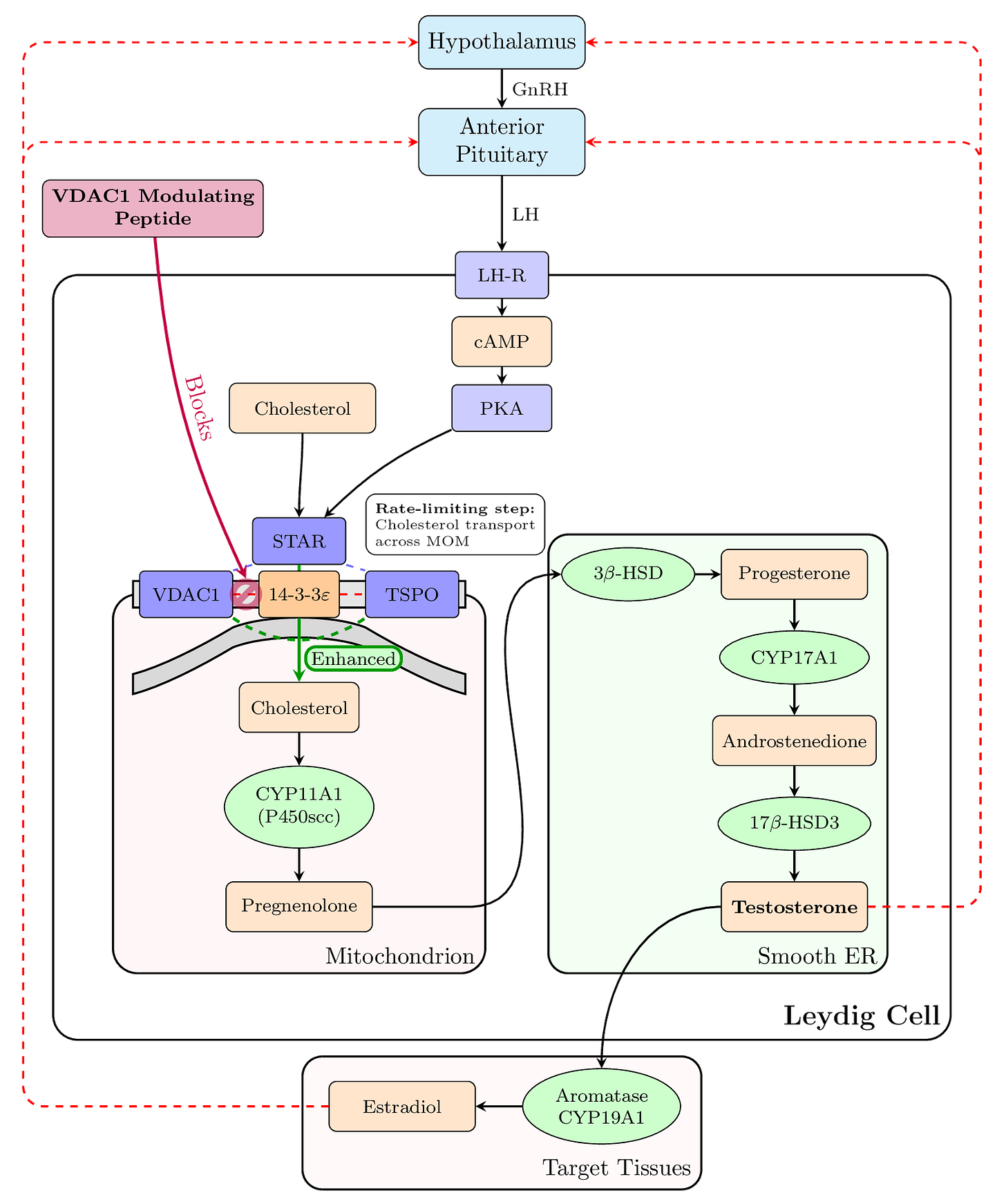
ACE-167 (Arg–D-Val–Thr–Gln): Compact and simple, but fast-acting.
N163-166 Mod. 6 (Ac–Arg–Ile–Thr–Gln–D-Ser–NH₂): A more durable version designed to resist breakdown in the body.
Both elevated testosterone in rats, by as much as 100%, without bypassing the body’s normal feedback control.
The N-of-1 Human Trial: Science, but Personal
Instead of jumping straight to a large clinical trial, this project starts small, just one participant. Me.
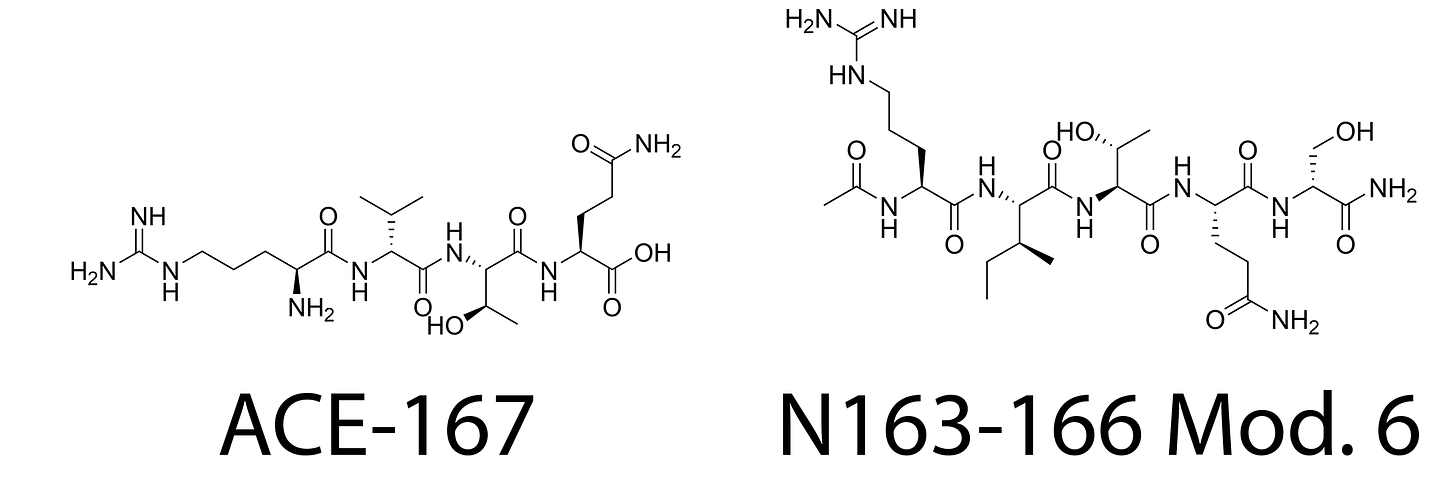
The single-participant (“N-of-1”) design includes three 14-day phases:
ACE-167
N163-166 Mod. 6
Placebo
The order is randomized and double-blinded. I won’t know which I’m receiving during each phase.
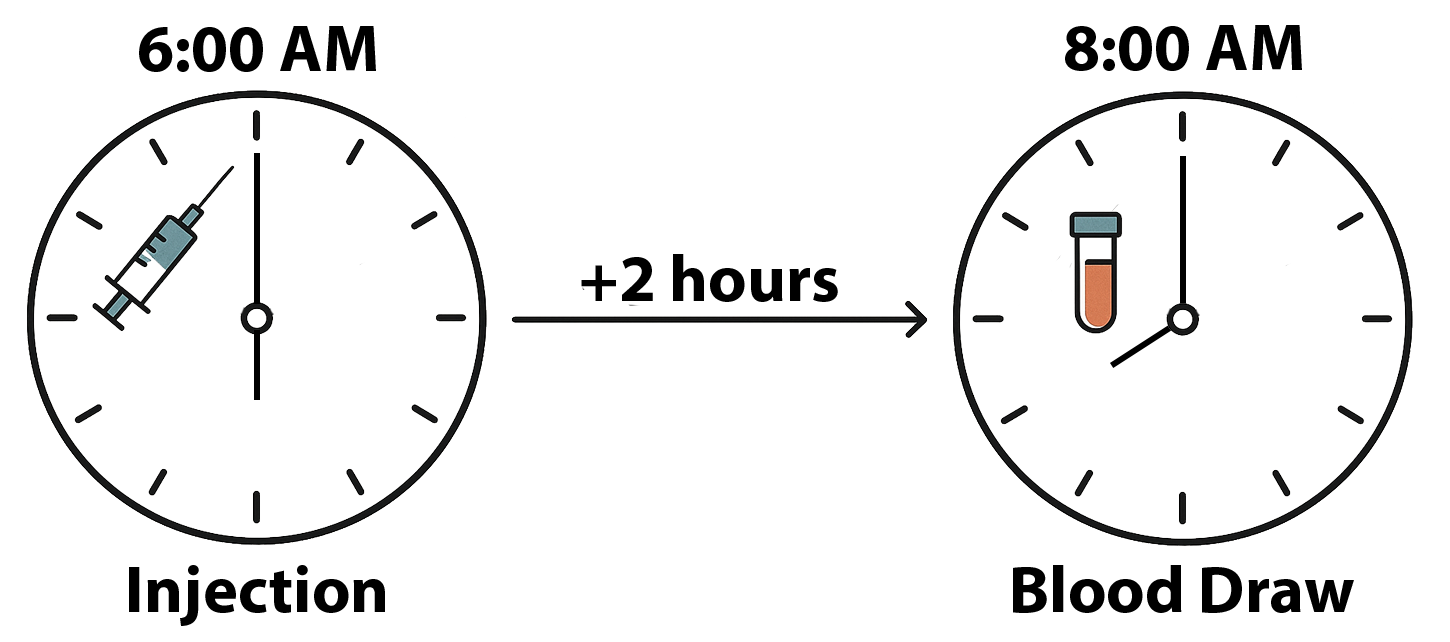
Every morning, I inject 30 micrograms subcutaneously right after waking, then have blood drawn two hours later on the first and last days of the phase. Testosterone, free testosterone, LH, estradiol, and SHBG are all measured using LC-MS/MS, the gold-standard assay for hormone analysis.
The Goal: A Meaningful Boost Without Replacement
The central question isn’t just “did testosterone go up?” but whether it rose enough to matter. The minimal clinically important difference (MCID) is set at roughly a 25% increase or +236 ng/dL over baseline; large enough to produce noticeable effects on energy, mood, libido, or performance.
The study also asks how this change happens:
Does LH decrease while testosterone rises (signaling the testicular machinery is more efficient)?
Does the testosterone-to-LH ratio improve?
Does free testosterone rise more than total testosterone?
Those patterns reveal whether the peptides are genuinely improving the body’s own steroidogenesis rather than simply altering downstream hormones.
Lifestyle Locked Down
To reduce noise in the data, everything else is controlled:
Sleep: consistent wake-up times within 30 minutes
No alcohol or caffeine before tests
Stable diet and exercise
All labs at 8:00 AM, at the same facility each time
This level of standardization ensures any hormonal change can be attributed to the peptides, not day-to-day variability.
The Analysis: Blending Old and New Statistics
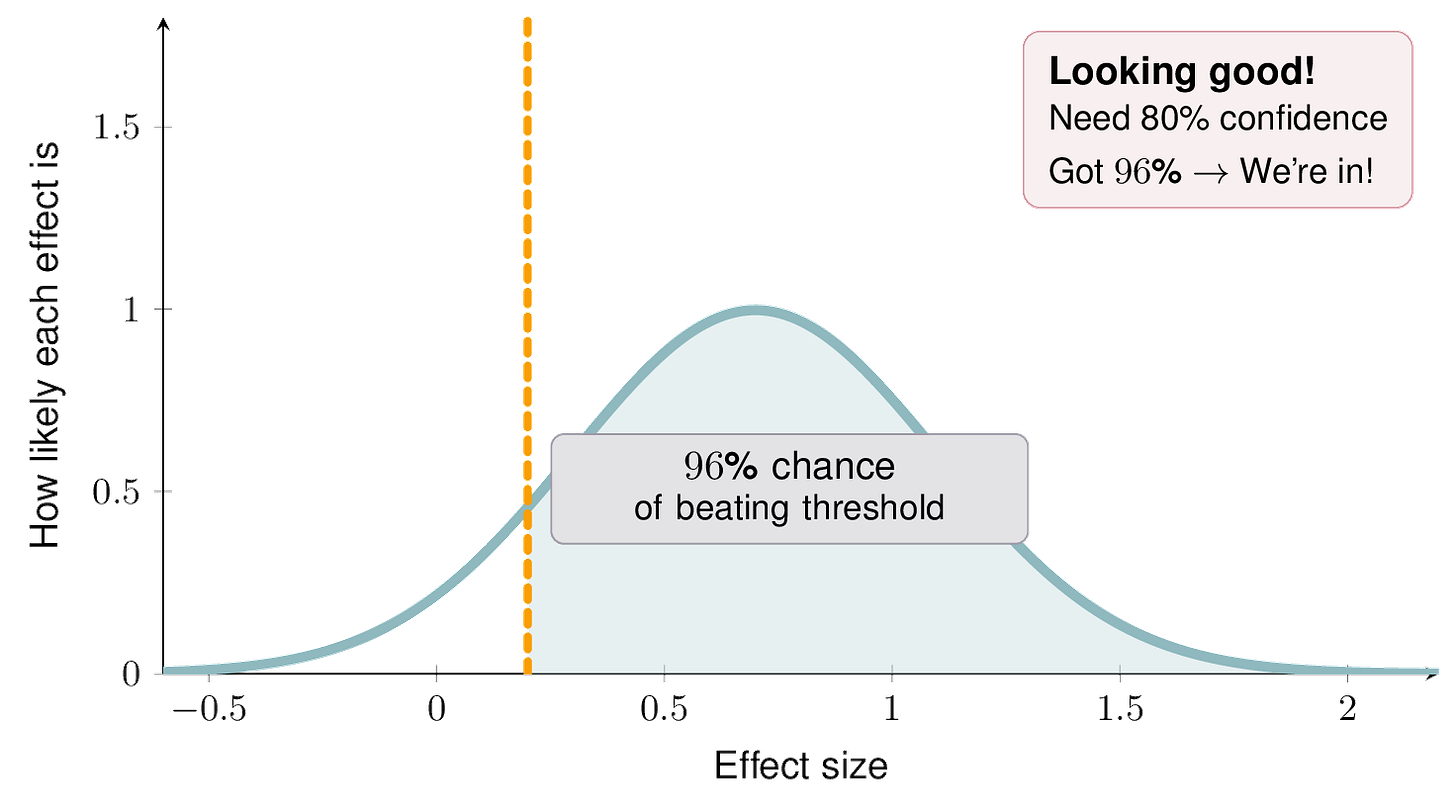
Results will be analyzed using both frequentist permutation testing and Bayesian hierarchical modeling. The Bayesian approach allows a probabilistic statement like:
“There’s an 80% chance the peptide raised testosterone by more than 25%.”
That 0.80 probability threshold serves as the decision point for declaring a pharmacodynamic effect.
Why This Matters
If VDAC1-targeting peptides can safely increase testosterone without suppressing the body’s own production, they could represent a new category of precision endocrine therapy; one that enhances hormone output from within rather than replacing it externally.
Instead of injecting testosterone and shutting down natural production, these peptides might allow a gentler, more physiological boost.
What’s Next
This experiment is a first step. If clear effects appear, the next phase could include:
A small series of replicated N-of-1 trials (5–10 participants)
Bayesian synthesis of results across individuals
A follow-up dose-ranging study
Eventually, a small randomized crossover comparing peptides to low-dose testosterone therapy or SERMs
All data and analysis code will be released publicly once complete to ensure transparency and reproducibility.
Final Thought
This project explores a new angle on hormone optimization: not by overwhelming the body with hormones, but by fine-tuning the machinery that makes them. It’s a bottom-up approach to restoring balance, starting from the mitochondria outward.
See below for the full experimental outline and protocol. Peptide synthesis and supply was provided by Upgraded Bio (admin@upgraded.bio).